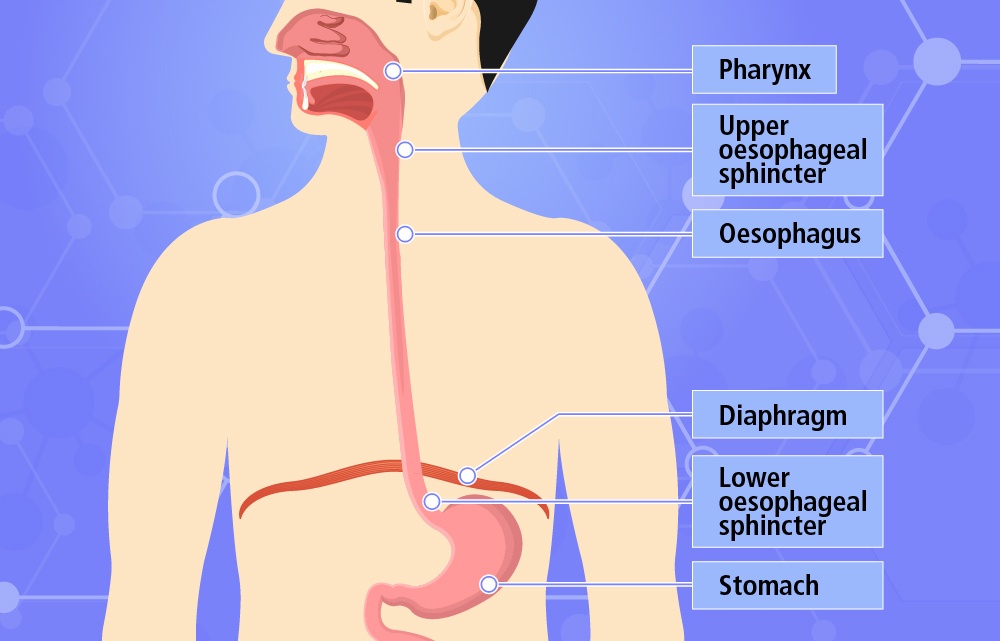
Chemotherapy plays a vital role in the treatment of oesophagus cancer, a type of malignancy affecting the oesophagus—the muscular tube connecting the throat and stomach. In this comprehensive guide, we will explore the various aspects of chemotherapy as a treatment modality for oesophagus cancer. From understanding the types of chemotherapy drugs used to examining its role as a primary, neoadjuvant, or adjuvant treatment, we will delve into the benefits, side effects, monitoring, and emerging advances in chemotherapy. By providing valuable insights, this article aims to empower patients and their families with knowledge to make informed decisions about their oesophagus cancer treatment journey.
Introduction to Chemotherapy in Oesophagus Cancer Treatment
Chemotherapy involves the use of powerful medications to target and destroy cancer cells. In oesophagus cancer treatment, chemotherapy can be employed as a primary treatment to shrink tumors before surgery, as neoadjuvant therapy, or after surgery to eliminate residual cancer cells, as adjuvant therapy. Additionally, chemotherapy may be combined with radiation therapy for enhanced efficacy. Understanding the role of chemotherapy in the overall treatment plan is crucial for patients and healthcare providers alike.
Types of Chemotherapy Drugs Used for Oesophagus Cancer
Several chemotherapy drugs are utilized in the treatment of oesophagus cancer, either as single agents or in combination regimens. Commonly used drugs include platinum-based drugs (such as cisplatin or oxaliplatin), fluorouracil (5-FU), taxanes (paclitaxel or docetaxel), and anthracyclines (such as epirubicin). Each drug works through different mechanisms to inhibit cancer cell growth and division. The choice of chemotherapy drugs depends on various factors, including the stage and location of the cancer, the patient's overall health, and potential drug interactions.
Chemotherapy as a Primary Treatment for Oesophagus Cancer
In some cases, chemotherapy may be administered as the primary treatment for oesophagus cancer, particularly if the tumor is inoperable or if the patient's overall health condition does not allow for surgery. This approach aims to shrink the tumor, alleviate symptoms, and improve overall quality of life. Chemotherapy may be used alone or in combination with radiation therapy in this setting. The treatment plan is individualized based on the patient's specific circumstances and medical team's recommendations.
Neoadjuvant Chemotherapy for Oesophagus Cancer
Neoadjuvant chemotherapy is administered before surgery with the goal of reducing the size of the tumor and increasing the likelihood of successful surgical outcomes. This approach can help downstage the cancer, making it more operable and potentially increasing the chances of complete tumor removal. Neoadjuvant chemotherapy regimens are typically delivered over a specific number of cycles before surgery, allowing time for the drugs to exert their effects. The decision to recommend neoadjuvant chemotherapy is based on factors such as tumor stage, location, and the patient's overall health.
Adjuvant Chemotherapy in Oesophagus Cancer Treatment
Following surgery for oesophagus cancer, adjuvant chemotherapy may be recommended to eliminate any remaining cancer cells and reduce the risk of cancer recurrence. Adjuvant chemotherapy is typically administered after the surgical procedure and may involve the same or different chemotherapy drugs used in the neoadjuvant setting. The duration and number of cycles of adjuvant chemotherapy depend on the patient's condition and the medical team's assessment of the potential benefits. This approach aims to improve long-term outcomes and reduce the risk of cancer spreading or returning.
Chemotherapy Combined with Radiation Therapy for Oesophagus Cancer
Combining chemotherapy with radiation therapy, known as chemoradiotherapy, is a common approach in oesophagus cancer treatment. This combined treatment approach helps to increase the effectiveness of both modalities. Chemotherapy can make cancer cells more sensitive to radiation, allowing for improved tumor control and potentially better long-term outcomes. The combination of chemotherapy and radiation therapy may be used in various treatment settings, including as a primary treatment for inoperable cancers or as a neoadjuvant or adjuvant treatment in conjunction with surgery.
Chemotherapy Side Effects and Management
Chemotherapy drugs can have side effects due to their impact on both cancerous and healthy cells. Common side effects include nausea, vomiting, hair loss, fatigue, decreased blood cell counts, and gastrointestinal issues. However, it's important to note that not all patients will experience the same side effects, and the severity can vary. Healthcare providers will closely monitor patients during treatment and provide supportive care to manage and alleviate side effects. Medications, dietary adjustments, and lifestyle modifications may be recommended to help patients cope with chemotherapy-related side effects.
Chemotherapy Regimens for Oesophagus Cancer
The choice of chemotherapy regimens for oesophagus cancer depends on several factors, including the stage of the cancer, the patient's overall health, and the medical team's expertise. Various combinations of chemotherapy drugs are used, and the treatment regimen is individualized for each patient. Common chemotherapy regimens include FLOT (fluorouracil, leucovorin, oxaliplatin, and docetaxel), ECF/ECX (epirubicin, cisplatin, and fluorouracil/capecitabine), and DCF (docetaxel, cisplatin, and fluorouracil). The selection of the most appropriate chemotherapy regimen is determined through a collaborative decision-making process between the patient and their healthcare team.
Monitoring and Response Assessment during Chemotherapy
During chemotherapy treatment, patients will undergo regular monitoring and assessment to evaluate the response to therapy. Imaging tests, such as computed tomography (CT) scans, may be performed to assess tumor size and response. Blood tests, including complete blood counts, may be conducted to monitor for any changes in blood cell counts. These assessments help healthcare providers determine the effectiveness of chemotherapy and make any necessary adjustments to the treatment plan.
Emerging Advances in Chemotherapy for Oesophagus Cancer
Advancements in cancer research have led to the development of new chemotherapy drugs and treatment strategies for oesophagus cancer. Targeted therapies, such as immune checkpoint inhibitors, are being explored to harness the body's immune system in fighting cancer cells. Clinical trials are ongoing to investigate novel chemotherapy agents, combination therapies, and personalized treatment approaches. These advancements hold promise for improving treatment outcomes and quality of life for patients with oesophagus cancer.
Conclusion
In conclusion, gastrointestinal stromal tumors (GISTs) are a significant area of concern in the field of gastrointestinal surgery. The expertise and dedication of professionals like Mr Nima Abbassi-Ghadi, a Consultant Laparoscopic/Robotic Gastro-intestinal Surgeon, are crucial in effectively managing and treating these tumors. Based in Guildford, Mr Abbassi-Ghadi serves both the NHS at the Royal Surrey County Hospital and private patients at the BMI Mount Alvernia and Guildford Nuffield Hospital.
GISTs are complex tumors that require specialized surgical techniques, and Mr Abbassi-Ghadi's extensive experience in laparoscopic and robotic gastrointestinal surgery positions him as a highly skilled practitioner in this field. Through his practice, he provides comprehensive care and the latest advancements in surgical approaches to ensure the best possible outcomes for his patients with GISTs.
By offering his services at multiple healthcare institutions, Mr Abbassi-Ghadi demonstrates a commitment to reaching a broader patient population and making his expertise accessible to those in need. His affiliation with the Royal Surrey County Hospital and private hospitals like BMI Mount Alvernia and Guildford Nuffield Hospital underscores his dedication to providing exceptional care in both public and private healthcare settings.
In conclusion, Mr Nima Abbassi-Ghadi's role as a Consultant Laparoscopic/Robotic Gastro-intestinal Surgeon, working at esteemed medical facilities and serving patients in Guildford, signifies the importance of specialized expertise in addressing gastrointestinal stromal tumors. His commitment to staying at the forefront of surgical advancements ensures that patients with GISTs receive the highest quality of care, leading to improved outcomes and a better quality of life.

No comments yet